by Karen Horney Clinic | Apr 18, 2017 | blog
A Norwegian study released in January looked at 700 children and the effects that exercise had on them when it came to depression. The

researchers looked at kids ages 6, 8 and ten years old over a four-year period and discovered that kids who got regular moderate-to-vigorous exercise were less likely to develop depression.
Previous studies evaluating physical activity and depression in adolescents and adults have found similar findings, but per the researchers, at the Norwegian University of Science and Technology, this is the first time this is suggested in children.
The study raises two questions. First, can physical activity be used to treat children who have depression, and second, can physical activity in children prevent depression. More studies certainly are needed for more definitive answers on the relationship between physical activity and depression, but what we can take away from this study is the mere fact that we have one more reason to keep kids active.
Here are some things that parents can do to keep their children active:
- Encourage your child to join a sports team at school and to put their best effort into gym class. Remind them that joining an intramural sport is as good as participating in a team.
- Encourage kids to get active after school. Bike riding, skateboarding, a good-ole fashion pick-up baseball game or just playing outside are all positive ways to keep kids active.
- Discourage kids from coming right in after school and going to watch television or get on the computer.
- Make sure to set a good example. Children often watch what their parents do. Get outside with them and throw a ball, play hop-scotch, go to the track and run with your son, or bike ride with your daughter.
- Have children help with chores. When it snows get them out with a snow shovel. Encourage them to help with yard work. Have them help wash the car, bring in the groceries and vacuum. And when they run out of things to do at home, surely grandma has something they can do.
The Center for Disease Control (CDC) also has guidelines for keeping kids active. You can read them here.
One final note, this study should not scare parents into worrying about their child becoming depressed if they don’t get enough exercise. According to the study, lack of exercise is not a precursor to depression. Also, we should remember exercise is a short-term fix as the majority of depressed children are usually caught up in unsolvable family conflicts or are being treated in a way that induces depression in the first place. Some sort of therapy is a must.
Click here to read the study published in Pediatrics, January 2017.
DISCLAIMER
The information contained in this blog is intended for educational purposes only. It is not intended as medical or psychiatric advice for individual conditions or treatment and does not substitute for a medical or psychiatric examination. A psychiatrist must make a determination about any treatment or prescription.

by Karen Horney Clinic | Apr 5, 2017 | blog
Tanning, because of its association with skin cancer, is a dangerous behavior. A new Yale School of Public Health (YSPH) study out in March is adding a new concern related to tanning. The YSPH study is saying that tanning may also lead to “other addictive behaviors.”
Published in the Journal of European Academy of Dermatology and Venereology, the study surveyed 499 white, non-Hispanic males, and females who had previously tanned indoors or outdoors. The study revealed, “participants who were tanning dependent were six times as likely to be dependent on alcohol, five times more likely to exhibit ‘exercise addiction,’ and three times as likely to suffer from Seasonal Affective Disorder (SAD).”

Photo courtesy of RF123
Addiction involves an intense craving for something, and the need to use it supersedes the negative effects or adverse consequences. Addiction is believed to be rooted in a change in the brain structure and function caused over time as the brain goes through a series of changes in response to recognition of pleasure. The brain then seeks this pleasure and creates a drive toward the compulsive behavior that becomes the addiction.
Tanning is dangerous and currently many states are enacting legislation to protect young people. The associated risk between tanning beds and skin cancer is strong. The Melanoma Foundation says tanning “increases the risk of melanoma associated with tanning bed use 59% for people whose first exposure to artificial UV rays in a tanning bed occurred before age 35 years. That risk increases with the number of tanning bed sessions per year. Melanoma, the deadliest form of skin cancer, kills one person every 50 minutes.”
Even though tanning beds are known to be dangerous many continue to use them still, and according to the study, the users are exhibiting a dependency to tanning. Researchers say that the connections between tanning dependence and other disorders revealed by the study represent an opportunity for clinicians to address those related conditions.
Yale Study
The Dangers of Tanning
DISCLAIMER
Information contained in this blog is intended for educational purposes only. It is not intended as medical or psychiatric advice for individual conditions or treatment and does not substitute for a medical or psychiatric examination. A psychiatrist must make a determination about any treatment or prescription.

by Karen Horney Clinic | Mar 29, 2017 | blog

HealthDay (3/15, Reinberg) reports that mixing opioid pain analgesics with benzodiazepine medications may be “a prescription for a deadly overdose,” researchers concluded after examining data on some “300,000 privately insured patients.”
The study published on March 14, 2017, in the British Medical Journal (BMJ), sought to identify trends in the concurrent use of benzodiazepine and an opioid. Data collected from 2001 to 2013 looked at the impact of mixing these drugs on admissions to hospitals and emergency rooms for opioid overdose. The study concluded that “concurrent benzodiazepine/opioid use sharply increased in a large sample of privately insured patients in the US and significantly contributed to the overall population risk of opioid overdose.”
Benzodiazepines (benzos) are a class of psychoactive drugs that work on the central nervous system and are used to treat a range of conditions including anxiety and insomnia. These drugs work by enhancing the effect of the neurotransmitter gamma-aminobutyric acid (GABA). They are responsible for reducing the activity of neurons that cause stress and anxiety. These drugs are generally safe and efficient for short-term use. However, benzos can be habit-forming, and the risks of long-term use are still being debated.
The more commonly prescribed benzos include Alprazolam (e.g., Xanax), lorazepam (e.g., Ativan), clonazepam (e.g., Klonopin), diazepam (e.g., Valium), and temazepam (e.g., Restoril) are the five most prescribed
Opioid addiction is at an epidemic level in the United States and in a December 2014 Express Script report it is estimated that 80 percent of the drugs are consumed by Americans. Opioids work by blocking pain signals to the brain. The more commonly known and prescribed painkillers include codeine, morphine, OxyContin® (oxycodone HCI), and Vicodin® (hydrocodone bitartate and acetaminophen).
“Nearly 60% of patients using opioids were taking a combination of drugs that are dangerous and potentially fatal; among these mixtures, almost one in three patients were prescribed anti-anxiety drugs known as benzodiazepines along with an opioid – the most common cause of overdose deaths involving multiple drugs,” the report (pdf), published by pharmacy benefit manager Express Scripts, said. [1]
The immediate risk of excessive use of benzos is the chance that they will be used in combination with alcohol or other drugs like opioids and cause an accidental overdose. Per the report, benzodiazepines have received less public safety attention than opioids, the combination of the two drugs is dangerous because benzodiazepines potentiate the respiratory depressant effects of opioids.[2]
Medical professionals need to make sure that patients fully understand the side effects of the drugs they are taking and the potential dangers of mixing these drugs with other drugs and alcohol.
DISCLAIMER
Information contained in this blog is intended for educational purposes only. It is not intended as medical or psychiatric advice for individual conditions or treatment and does not substitute for a medical or psychiatric examination. A psychiatrist must make a determination about any treatment or prescription.
[1] “U.S.: 5% of World Population; 80% of Opioid Consumption.” Express Script Report December 2014. N.p., n.d. Web. 26 Mar. 2017 %3chttp:/www.allgov.com/news/controversies/us-5-percent-of-world-population-80-per%3e
[2] “Association between concurrent use of prescription opioids …” BMJ.com. N.p., n.d. Web. 26 Mar. 2017 %3chttp:/www.bmj.com/content/356/bmj.j760%3e

by Karen Horney Clinic | Mar 11, 2017 | blog
This month Aetna joined fellow insurers Anthem and Cigna in dropping the prior authorization requirement for privately insured patients to prescribe “particular medications ― such as Suboxone ― that are used to mitigate withdrawal symptoms.” Aetna is the third leading health care insurer to drop the pre-authorization in recent months.
 Opioid abuse in the United States is a serious public health issue and drug overdose deaths involving opioids and heroin continue to sweep across the country at epidemic proportions. Suboxone is one of several drugs used to treat narcotic (opiate) addiction. To medical professionals, addiction specialists, and families of loved ones addicted to opioids and heroin, the pre-authorization that insurers currently have in place is a barrier to timely and effective treatment.
Opioid abuse in the United States is a serious public health issue and drug overdose deaths involving opioids and heroin continue to sweep across the country at epidemic proportions. Suboxone is one of several drugs used to treat narcotic (opiate) addiction. To medical professionals, addiction specialists, and families of loved ones addicted to opioids and heroin, the pre-authorization that insurers currently have in place is a barrier to timely and effective treatment.
“This is great news,” says Dr. Henry Paul, Executive Director of the Karen Horney Clinic in NYC. “When a patient decides right then and there that they want treatment to kick their addiction, you need to begin treatment at that moment. The window of opportunity to treat patients who want to kick their addiction is minuscule and you can’t send them away expecting they’ll come back tomorrow. By then they will be back using because the craving for the drugs is just too powerful.”
In February NPR reported on Aetna’s change saying, “Specifically, the company will stop requiring doctors to seek approval from the insurance company before they prescribe particular medications ― such as Suboxone ― that are used to ease withdrawal symptoms.”
So how long were the pre-authorization delays? Sometimes hours and sometimes days. Pre-authorization may seem like a simple technicality but any delay, however brief, puts a person’s ability to get well at risk.
Both Cigna and Anthem changed their policy after facing an investigation by New York’s Attorney General in to whether their coverage practices unfairly barred patients from needed treatment. Aetna’s change takes effect this month and it is expected that more states will begin their own investigations and other insurers will follow suit and drop their pre-authorization requirement.
Another Big Health Insurer Loosens Rules For Covering Addiction Treatment (NPR News, 2/15/2017)
Facing Pressure, Insurance Plans Loosen Rules For Covering Addiction Treatment (KHN, 2/21/2017)
DISCLAIMER
Information contained in this blog is intended for educational purposes only. It is not intended as medical or psychiatric advice for individual conditions or treatment and does not substitute for a medical or psychiatric examination. A psychiatrist must make a determination about any treatment or prescription.
by Karen Horney Clinic | Mar 7, 2017 | blog
“There is no good reason why we should not develop and change until the last day we live.”
― Karen Horney, MD
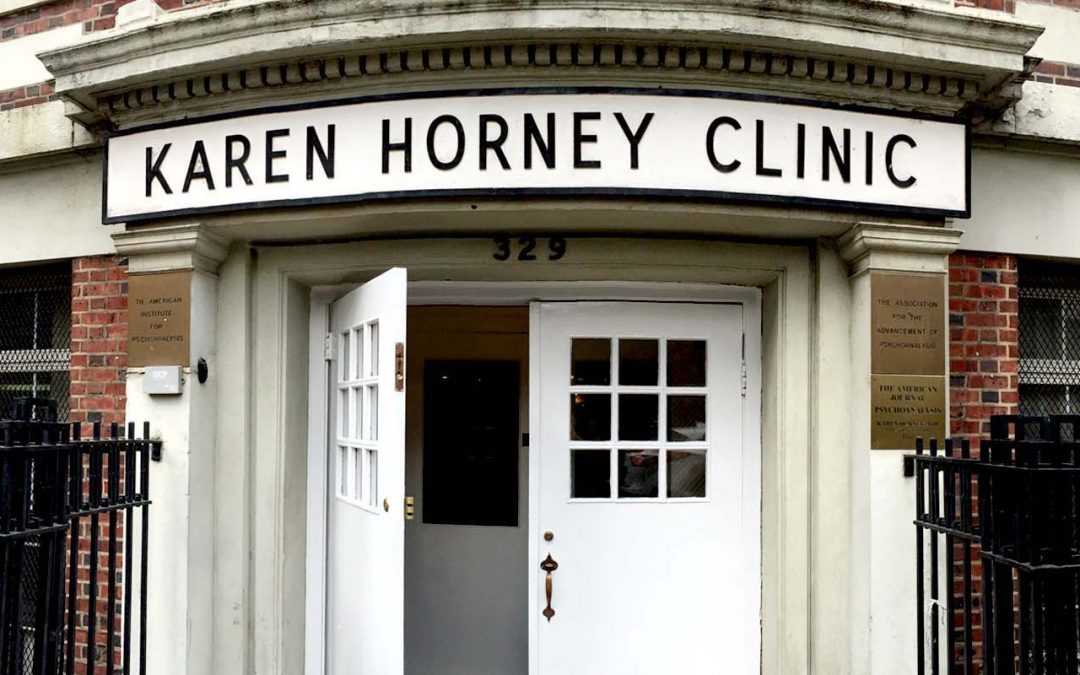
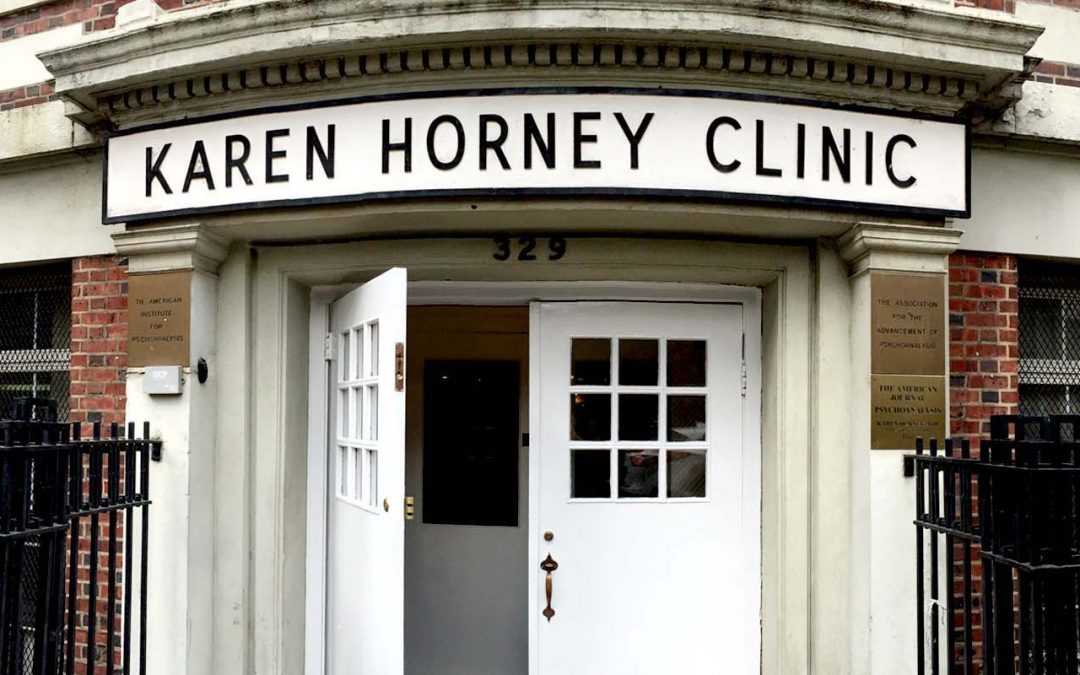
The Karen Horney Clinic was founded in 1955 in honor of Karen Horney, MD, a pioneer in the field of psychoanalysis. The clinic’s mission 
has always been to offer low-cost psychoanalytic and psychotherapeutic services and to provide training and research opportunities for advanced mental health professionals.
The Karen Horney Clinic is a vital center for mental health treatment, training, and research in New York City. Meeting the mental health needs of a diverse community the clinic continually evolves and expands its services providing New Yorkers, from all backgrounds, the most professional and compassionate mental health care at an affordable cost.
A not-for-profit organization Licensed by the New York State Office of Mental Health, the Karen Horney Clinic is funded through a combination of private contributions, foundation and government grants, and offers a sliding scale fee based on an individual’s ability to pay and Medicare, Medicaid, and numerous other insurances are accepted.
The Karen Horney Clinic also provides advanced training in psychodynamic and psychoanalytic therapy for graduates of doctoral, social work and mental health counseling programs.
Who Is Karen Horney?
 A pioneer in psychoanalysis, Karen Horney was a visionary who questioned the role of gender in the development of the neurotic personality as well as the importance of society and culture as determining and gauging factors for normal and pathological development.
A pioneer in psychoanalysis, Karen Horney was a visionary who questioned the role of gender in the development of the neurotic personality as well as the importance of society and culture as determining and gauging factors for normal and pathological development.
Horney’s advanced theories regarding neurosis and personality led her in 1937 to publish the popularly read book, “The Neurotic Personality of Our Time.” She founded the Association for the Advancement of Psychoanalysis and the American Institute for Psychoanalysis. Horney founded these organizations because she was dissatisfied with the generally strict, orthodox nature of the psychoanalytic community. She is the only female founder of a psychoanalytic school of thought.
Services
The Karen Horney Clinic offers mental health treatment to adults, children and their families and caregivers, those who have suffered a trauma, and young adults who are adjusting to student life in a demanding academic environment.
Therapeutic services include treating a broad range of emotional and mental health concerns, including depression, anxiety, psychosomatic disorders, phobias, personality problems, sleep disturbance, obsessive compulsive disorder, family problems, stage of life issues, and post-traumatic stress to mention only a few.
Services particularly geared for children include early intervention in cases of childhood problems including failure at school, violence, parent-child issues, bullying, cyber bullying and social network abuses, behavioral disturbances, depression, anxiety, and drug and alcohol abuse. The clinic also helps to prevent damaging psychological effects on children who were removed from their parents for abuse and neglect and placed in foster care. The clinic’s highly individualized treatment is designed for each child and their family.
For more information on The Karen Horney Clinic visit www.karenhorneyclinic.org or call 212-838-4333. The clinic is open Monday through Friday 9:00 AM to 9:00 PM and is located at 329 E. 62nd Street, New York, NY 10065.
DISCLAIMER
Information contained in this blog is intended for educational purposes only. It is not intended as medical or psychiatric advice for individual conditions or treatment and does not substitute for a medical or psychiatric examination. A psychiatrist must make a determination about any treatment or prescription.